The evaluation of the female cycle and of fertility is based on 2 pillars:
- The hormonal determination of the anti-Müllerian hormone at any time of the cycle (AMH), but also of other hormones such as FSH (follicle-stimulating hormone), LH (luteal-stimulating hormone), Estradiol and Progesterone.
- The antral follicle count by transvaginal ultrasound.
FSH and LH are the stimulating hormones responsible for stimulating activity in the ovaries and are produced in the central nervous system. Both FSH and LH are transported to the ovary, where they stimulate the development of follicles and the maturation of oocytes throughout the woman’s cycle.
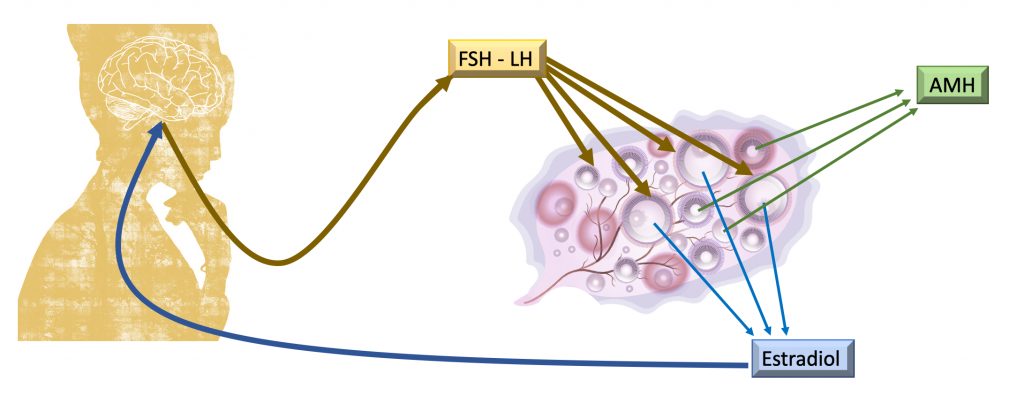
In a natural cycle of women, there are multiple follicles that initially respond to the stimulation made by FSH and LH, however, from a critical moment, only one of the follicles continues its growth and maturation. The rest of the follicles will degenerate and disappear. This selected follicle will continue to grow throughout the cycle and, as it grows, it will produce estradiol.
When the follicle reaches maturity, ovulation will take place and then the production of another hormone, progesterone, will begin, responsible for allowing pregnancy in the second phase of the cycle.
Estradiol and progesterone reach different organs to develop the sexual characteristics of women and also regulate the secretion of other hormones (FSH and LH). That is, the ovary itself is also capable of self-regulating its activity, indirectly. Thus, the measurement of estradiol, FSH and LH in the first phase of a menstrual cycle, will assess the activity of the ovary in a given cycle.
It is important to emphasize that this hormonal profile varies throughout the cycle, from one cycle to another in the same woman or with intake of contraceptives and is also very sensitive to age, so its evaluation must be very cautious to avoid diagnostic errors.
The normal values of these hormones may vary from one lab to another, but they should be within these ranges:
| FOLLICULAR PHASE | OVULATORY PHASE | LUTEAL PHASE | MENOPAUSE | |
| FSH | 2-10 UI/l | 8-20 UI/l | 2-8 UI/l | >20 UI/l |
| LH | 2-6 UI/l | 6-20 UI/l | 3-8 UI/l | >30 UI/l |
| ESTRADIOL | 20-120 pg/ml | 90-450 pg/ml | 50-300 pg/ml | <20 pg/ml |
| PROGESTERONE | 0-1.40 ng/mL | 4-30 ng/mL | 4-30 ng/mL | <1 ng/mL |
Anti-Müllerian Hormone (AMH) is a hormone that can be measured in the blood and is produced by the small ovarian follicles in the ovaries, that is, those that have not yet been selected.
Its blood level, therefore, is indicative of the number of small follicles that exist in a woman’s ovary, known as the ovarian reserve.
The advantage of using antimüllerian hormone is that its value does not change significantly throughout the cycle or from one cycle to another, so we can measure it at any time to assess the patient’s ovarian reserve.
The value of AMH before an in vitro fertilization cycle has prognostic value, since it predicts the response that we can expect from ovarian stimulation in each woman and allows us to select the dose of medication and the type of protocol in each case.
Normally, AMH values decrease with the age of the patient, but they are also very low in young women with a highly compromised ovarian reserve.
The AMH and antral follicle count (AFC) are the most widely used ovarian reserve markers nowadays.